Sep, 2022
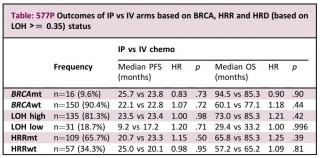
The iPocc randomised multicentre international study reported improved progression-free survival (PFS) but not overall survival (OS) with IP carboplatin and IV paclitaxel vs IV chemotherapy (chemo) in patients (pts) with epithelial ovarian, fallopian tube or primary peritoneal cancer. Previous studies suggested that pts with BRCA-deficient tumours may benefit from IP chemo. We conducted a non-prespecified analysis of the prognostic and predictive value of HRD in tissue samples retrospectively obtained from iPocc trial pts. 166 pts from participating centres in Singapore and Japan had adequate tissue for next-generation sequencing with ACT Genomics ACTOnco®+. HRD was defined by high loss of heterozygosity at a threshold of >=0.35 (LOH high) or presence of a pathogenic BRCA mutation (BRCAmt). Median PFS and OS were estimated using Kaplan-Meier method. Fisher’s exact and Student’s t-test were used to compare group characteristics. Both IP and IV arms had similar frequencies of BRCAmt, homologous recombination repair pathway mutations (HRRmt) and LOH high. All BRCAmt tumours were LOH high. There were no differences in PFS or OS in IP vs IV arms in this cohort. Outcome data based on HRD subgroups are summarised in the table. In the overall group, LOH high was associated with improved OS (HR 0.43, p=.001) but not PFS (HR 1.04, p=.87). BRCAmt pts showed a trend towards improved OS (HR 0.68, p=.24) and PFS (HR 0.73, p=.32). HRRmt status did not significantly affect OS (HR 0.95, p=.84) or PFS (HR 1.21, p=.30).